Blog Posts
Managing Sepsis Care using the EMR


Editor’s note: More than 40 hospitals and health systems clients presented at the recent Allscripts Client Experience (ACE) event held in Dallas, Texas. Here, a leader from Auburn Community Hospital discusses achieving exceptional Sepsis care.
Over the past few years, healthcare facilities nationwide have turned their focus to Sepsis. Sepsis strikes at least 1.7 million U.S. adults annually and is a contributing factor in one in every three hospital deaths.
Sepsis, at its inception, is difficult to recognize but easy to treat. If left unattended, however, it becomes easy to recognize but extremely difficult to treat.
Auburn Community Hospital (Auburn, NY) is beating the odds while setting the bar high for Sepsis management.
At the recent Allscripts Client Experience (ACE) conference, I detailed how Allscripts Paragon® EHR helps our physicians provide exceptional Sepsis care, especially for one at-risk patient in saving her life.
Due to its high mortality rate, mandatory reporting on ALL cases of Severe Sepsis and Septic Shock is required by CMS and the New York State Department of Health (NYSDOH).
Since reporting, Auburn has averaged one Sepsis case every other day, which is an alarming number for a small community hospital. This prevalence, combined with the high mortality rates associated with Sepsis, and the associated regulatory requirements, are why Sepsis management became a main priority for us at Auburn.
An outstanding real-world Sepsis case
An 86-year-old patient came into our ER one morning after choking on her breakfast. Her temperature was 95 degrees Fahrenheit/35 degrees Celsius, and she had a pulse of 46. According to the below CMS & NYSDOH criteria, a low pulse isn’t a Sepsis indicator.
Per the regulations, a patient meets SIRS (Systemic Inflammatory Response Syndrome – one part of Severe Sepsis) if they meet two or more of the below criteria:
- Temp > 38.3 C or < 36.0 C / >100.9 F or <96.8 F
- Heart rate > 90 bpm
- Respiratory rate > 20/minute
- WBC > 12K or < 4K
Many providers don’t assume Sepsis without a fever or high pulse. Fortunately, Auburn physician Dr. Shakeel Usmani immediately recognized Sepsis and began treatment by submitting our “ED Sepsis Pathway” in CPOE. The system enables us to pre-select necessary orders, such as lab tests like Blood Cultures and Lactic Acid. They may also uncheck any items that may not be applicable.
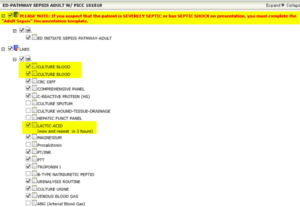
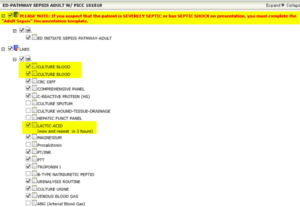
In the Paragon solution, we are able to build the Lactic Acid value as “Timed” so that a second draw can be obtained three hours after the first without the provider having to remember to place the second order. Other lab orders can be pre-built as “Once” and “Stat” to eliminate extra clicks for the Physicians.
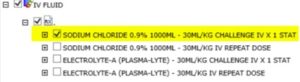
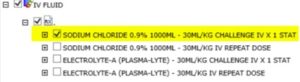
Based on audits I’ve performed, it seems that failure to administer IV fluid contributes to negative Sepsis outcomes. But in Paragon, we’ve built the evidence-based/recommended IV fluid options that the physician can select with one click.
Antibiotics to tackle source of infections made easy
Another requirement of CMS reporting involves antibiotic administration, as we must report if it was given on time and whether or not it was the correct selection. We included the appropriate antibiotics, by infection source, in the “ED Sepsis Pathway.” Additionally, we broke out the antibiotics into their own order set so that if the physician decides later that the patient has Sepsis, they can open up this order set alone and chose the correct antibiotic.
Ability to build custom Physician Documentation templates
The goal is not only to facilitate and remind providers of care, but also to capture the necessary data. I built a custom Physician Documentation template in Paragon that contains CMS/NYSDOH criteria, making documentation and data capture more efficient.
Because the patient developed Systemic Inflammatory Response Syndrome (SIRS) criteria for Organ Dysfunction, and blood pressure remained low after administration of fluid, the patient qualified for a diagnosis of Septic Shock. Dr. Usmani ordered additional fluid and Vasopressors to treat the persistent hypotension, as recommended by guidelines.
Within just a few hours, the patient was stabilized and admitted to the Intensive Care Unit. The patient was downgraded to a medical floor five days later and discharged home five days after.
While the patient didn’t meet all Severe Sepsis criteria on presentation, our physician immediately recognized several important precipitating factors and the likelihood of impending Sepsis. He used our customized Sepsis order set in CPOE to begin early interventions. He also used our custom Sepsis Physician Documentation note to follow through with reportable guidelines.
Hospitals can build systems in such a way to facilitate the physician workflow, provide the best care and save more lives.